HR+/HER2− Breast Cancer – What You Need to Know
If you’ve just heard the term HR+/HER2− while talking to a doctor, it can feel like a jumble of letters. In plain English, it means the cancer cells have hormone receptors (HR) that respond to estrogen or progesterone, but they don’t have extra HER2 proteins. This combo is actually the most common type of breast cancer, so there’s a lot of research and many treatment paths available.
Understanding the label helps you ask the right questions and follow a plan that fits your life. Below we break down how doctors find this subtype, what the numbers mean, and which therapies are most effective today.
How Doctors Diagnose and Stage HR+/HER2− Cancer
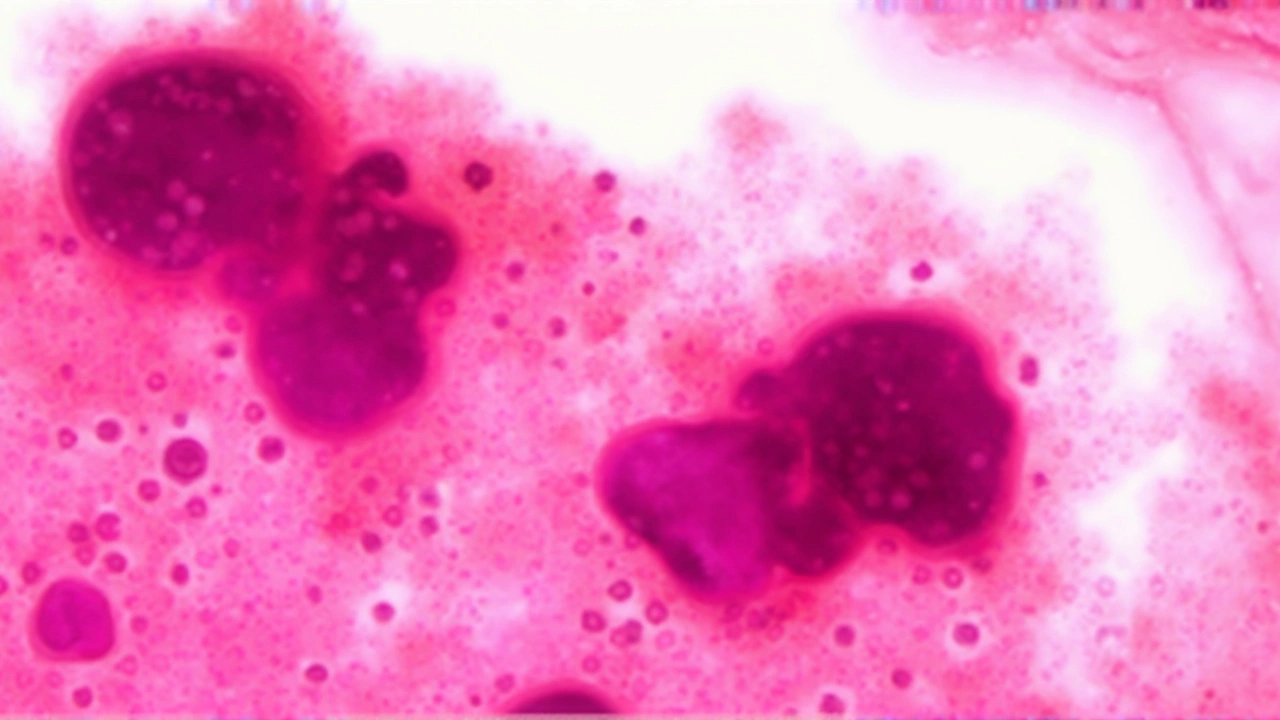
The first step is a biopsy. A tiny piece of tissue is taken from the tumor and examined under a microscope. Labs run tests called immunohistochemistry (IHC) to see if estrogen receptors (ER) or progesterone receptors (PR) are present. If they are, the cancer is “hormone‑receptor‑positive.” At the same time, another test checks for HER2 proteins. If HER2 is low or absent, you get the HR+/HER2− label.
Staging comes next. Doctors use imaging—mammograms, ultrasounds, MRIs, sometimes PET scans—to see how far the cancer has spread. Stages range from I (small, confined) to IV (spread to other organs). Your stage, combined with the HR/ HER2 status, determines which treatments are likely to work best.
Keep a copy of your pathology report. It’s the blueprint for your care, showing the exact percentage of cells that are ER/PR positive and the HER2 score. If anything looks unclear, ask your oncologist to walk through the numbers with you.
Treatment Options for HR+/HER2− Cancer
Because the tumor relies on hormones to grow, the cornerstone of therapy is hormone (or endocrine) treatment. Common drugs include tamoxifen, aromatase inhibitors (like letrozole, anastrozole, or exemestane), and newer agents such as CDK4/6 inhibitors (palbociclib, ribociclib, abemaciclib). These medicines either block the hormone receptors or lower estrogen levels in the body.
If the cancer is found early and is operable, surgery often comes first—either a lumpectomy (breast‑conserving) or a mastectomy. Radiation usually follows lumpectomy to clean up any leftover cells. After surgery, most patients get endocrine therapy for five to ten years to keep the cancer from coming back.
For larger or node‑positive tumors, doctors may add chemotherapy before surgery (neoadjuvant) to shrink the tumor, making the operation easier. Even though HR+ cancers tend to respond less dramatically to chemo than other types, it can still improve outcomes when the disease is advanced.
Targeted therapy with CDK4/6 inhibitors has changed the game for many patients with metastatic HR+/HER2− disease. When paired with an aromatase inhibitor, these drugs can delay progression for years and often have a manageable side‑effect profile.
Side effects vary. Hormone therapy can cause hot flashes, joint aches, or mood changes. CDK46 inhibitors may cause low blood counts or fatigue. Talk to your care team about ways to ease these—exercise, dietary tweaks, or prescription meds can help.
Finally, don’t overlook support. Joining a local breast cancer group, using online forums, or seeing a counselor can make a huge difference in coping with diagnosis, treatment decisions, and survivorship.
HR+/HER2− breast cancer is common, well studied, and treatable. By knowing what the label means, staying on top of your pathology report, and working closely with your medical team, you can navigate treatment with confidence and focus on what matters most—your health and life beyond cancer.